Ulcerative colitis
Medically Reviewed by Dr Aifric Boylan
Last updated on 26.06.2024
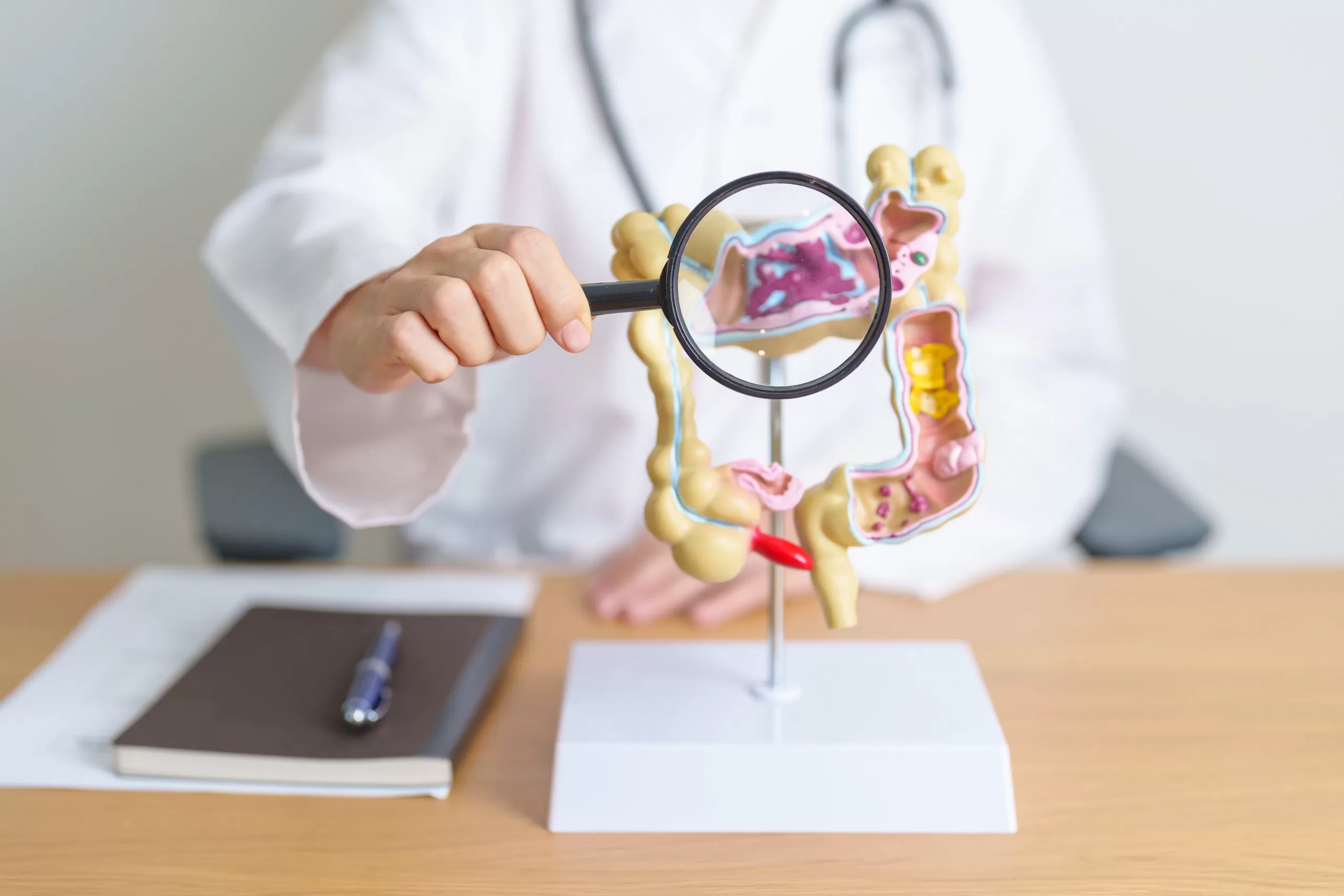
Ulcerative colitis (UC) is a condition where inflammation occurs in the large bowel (colon) and the rectum. It is one of two major inflammatory bowel diseases, the other being Crohn’s disease which can affect the whole gastrointestinal tract from the mouth to the anus.
UC is about three times more common than Crohn’s disease and affects approximately 1-5 people in 1,000. It is slightly more common in women than men and the peak incidence occurs between 18 and 40.
Causes and risk factors
The cause is unknown, but it is thought to be an autoimmune condition which means the body attacks the bowel. Some associations with UC include:
- Family history of UC or Crohn’s disease
- Medications, such as anti-inflammatories and antibiotics
- Infections, such as gastroenteritis caused by bacteria or viruses
- Not-smoking: smokers are less likely to get UC
- Psychological stressors, because these are known to suppress the immune system
- Other autoimmune conditions, because they often coexist in the same person
Symptoms of ulcerative colitis
Symptoms of ulcerative colitis can include:
- Rectal bleeding
- Abdominal pain
- Bloating
- Diarrhoea and frequent stools
- Mucus from rectum
- The feeling of not emptying your bowel fully
- Non-gastrointestinal symptoms, which can affect the eyes, joints and skin
Disease progression and complications
Symptoms can come and go, depending on how severe they are. Some people may have mild symptoms that can seem like gastroenteritis or haemorrhoids and so do not seek medical advice. Others can have UC that progresses and worsens, leading to complications in the bowel and hospitalisation. Severe UC that is untreated over time can lead to bowel cancer, because the chronic inflammation in the bowels affects how the cells there develop. This is an important reason why treatment of UC is necessary.
Diagnosis of ulcerative colitis
Ulcerative colitis is best diagnosed with a colonoscopy which is a procedure done while you are asleep. It involves a camera entering the anus and examining the rectum and large bowel. During the colonoscopy, small samples (biopsies) of the bowel are taken and then examined in a laboratory to help diagnose the condition. Other tests for UC can include:
- Blood tests
- Stool tests
- CT scan of your abdomen
Treatment of ulcerative colitis
Treatment of ulcerative colitis can be done as an outpatient if you have mild disease. If you are unwell and require hospitalisation, treatment can be commenced as an inpatient. This can include:
- Corticosteroids: these are anti-inflammatories that settle bowel disease. Generally speaking, this treatment is not prolonged because of side effects when taken too long, so is mostly used to stabilise UC. It can be given intravenously, orally or rectally.
- Aminosalicylates: these medications can cause remission of UC and can be given orally or rectally.
- Immunosuppressants: these work by suppressing the overactive immune system, so that UC can go into remission.
- Biologic agents: these are newer medications that are given intravenously or subcutaneously (superficial injection into fat) and can reverse UC and lead to long term remission. They are also immunosuppressants but work in a different way, tending to have less side effects. In order to access these medications, people with UC generally have to have tried a combination of the previously mentioned medications.
- Surgery: sometimes UC can lead to complications in the abdomen such as fistulas or abscesses, and these would require an operation.
Management of ulcerative colitis
Ulcerative colitis is considered a chronic condition and that means multidisciplinary treatment is ideal. This can include a psychologist, dietitian, GP and gastroenterologist. Because of the nature of the medications used for UC, you may also need to see other specialists over time if they affect your fertility, heart or kidneys.
If you have a healthy diet and lifestyle and have developed a successful medication regimen that controls your UC, you can live a fulfilling life without complications.
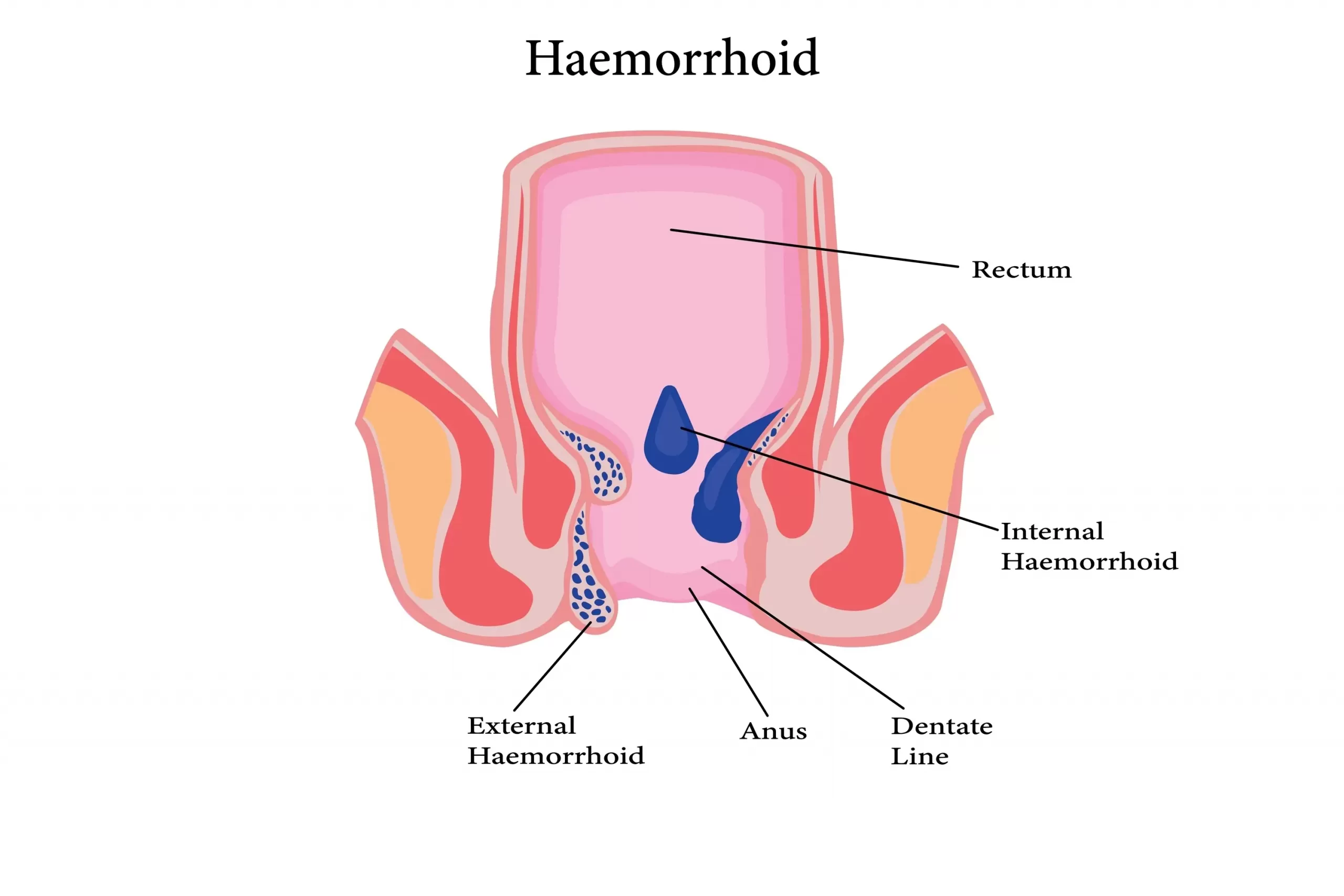
Haemorrhoids
Haemorrhoids Haemorrhoids, also known as piles, are a very common medical condition. The pelvis and anus have a lot of blood vessels, and around the rectum, some veins are [...]
Ulcerative colitis
Ulcerative colitis Ulcerative colitis (UC) is a condition where inflammation occurs in the large bowel (colon) and the rectum. It is one of two major inflammatory bowel diseases, the [...]
How to get rid of acid reflux
Acid reflux- causes and treatment Acid reflux is when stomach acid flows from the stomach upwards into the oesophagus. The oesophagus (us-off-a-gus) is the tube connecting your mouth with [...]