Balanitis: Signs, triggers, and how to treat it
Medically Reviewed by Dr AIFRIC BOYLAN
Last updated on 06.11.2025
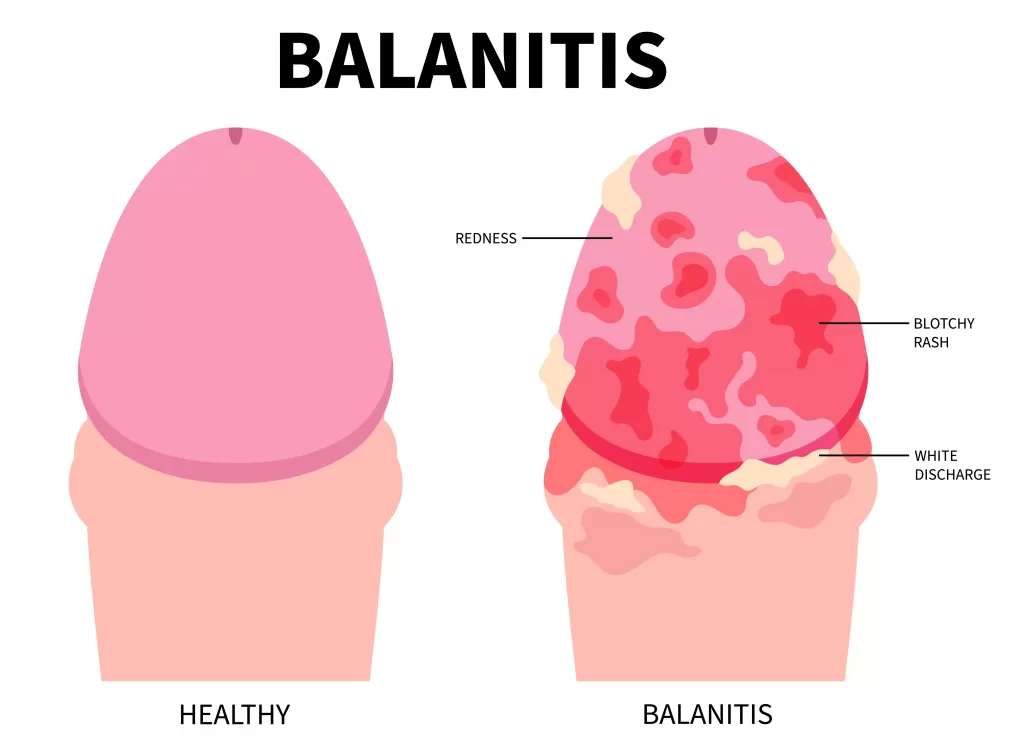
Balanitis is inflammation of the head of the penis (glans). It can cause symptoms such as irritation of the glans, redness, discomfort, swelling, small spots or discharge that is white and thick (or cheesy).
There are many causes of balanitis, including dermatitis, irritants, fungal infection, bacterial infection, physical rubbing, yeast infection, poor hygiene, and also overzealous cleaning.
Risk factors for balanitis
Balanitis is much more likely to occur in men who are uncircumcised because the glans is covered by the foreskin, which creates a moist, closed, and warm environment for bacteria and fungi to overgrow.
Balanoposthitis: A related condition
Another condition, balanoposthitis, means inflammation of the foreskin and glans, which has the same triggers and causes as balanitis.
Common triggers and causes of balanitis
- Diabetes: Particularly if your diabetes is poorly controlled, because the high amount of sugar in your blood allows fungi and bacteria to overgrow, plus your immune system is not able to function as well as usual.
- Soaps and shower gels: These clear all the good oil from the genitals, leaving the skin dry, irritated, and without the natural oil to protect it from bacteria and fungi that naturally live on the skin. The warm water in the shower also removes good oil from the skin, so after you leave the shower and dry with a towel, the skin has been stripped of all its protection.
- Phimosis: A tight foreskin that does not fully retract can trap urine and smegma (normal penile lubricant), creating a moist environment that irritates the head of the penis and can trigger balanitis.
- Oral antibiotics: Can affect the normal bacteria on the body, leading to an overgrowth of fungus or yeast on the penis.
- Irritation of the glans: Lubricants, cleansers, loofahs, latex, washing powders, sex, obesity, and other chemicals and physical irritants can inflame the glans.
- Drugs: Medications such as tetracyclines and sulfonamides.
- Viruses: Herpes simplex can cause balanitis, presenting with painful ulcers. However, other STIs like chlamydia and gonorrhoea are less likely to cause balanitis.
- Other skin conditions: Skin conditions like intertrigo, psoriasis, and lichen planus can affect the skin of the genitals, including the foreskin and glans.
Diagnosing balanitis
Balanitis is best diagnosed with a physical examination by your doctor. Sometimes they may decide to do a swab of the glans, particularly if there are ulcers. Blood tests may be required, for example, if diabetes is suspected.
Treatment options for balanitis
Treatment depends on the underlying condition, but generally, you would be advised to:
- Avoid overcleaning the penis with soap or shower gel, and use only water. Pat dry under the foreskin after showering. If you never clean under the foreskin, get into the habit of pulling the foreskin back and cleaning with water.
- If you are unable to pull the foreskin back to expose the glans fully, then steroid creams can help loosen the tight skin of phimosis, allowing appropriate cleaning with water.
- Use a cream with an antifungal and cortisone, applying it to the head before pulling the foreskin back down over the head. Creams are generally used 2-3 times per day for about two weeks, but this can be longer depending on the cause.
- Avoid triggers, lose weight, and improve your overall health with diet, exercise, sleep, and avoiding substance misuse.
- In rare instances where balanitis is recurrent and distressing, circumcision can be considered.
When to seek further medical advice
If you have balanitis, it can also provide an opportunity to discuss genital skin care, sexually transmitted diseases, and general sexual health with your doctor. More complicated cases may require you to see a dermatologist.
Weight loss programs: how to choose the right option in Australia
Weight loss programs: how to choose the right option in Australia Why many Australians choose Qoctor for weight loss support At Qoctor, we’re transparent about how our approach works, so people can [...]
Weight Loss Support Through Qoctor: A Doctor-Led Telehealth Approach
Weight Loss Support Through Qoctor: A Doctor-Led Telehealth Approach Weight loss is rarely just about weight alone. For many Australians, it is closely linked with overall health, lifestyle, mental wellbeing, and underlying [...]
Getting a Mental Health Care Plan in Australia: Your Guide
Getting a Mental Health Care Plan in Australia: Your Guide Mental health matters—and if you’re feeling overwhelmed, anxious, or down, a mental health care plan can help. But what is it, and how do [...]